How is dysphagia managed after a stroke?
If dysphagia is diagnosed, a dietitian may be consulted for advice on which types of food and drinks are easiest and safest to consume.
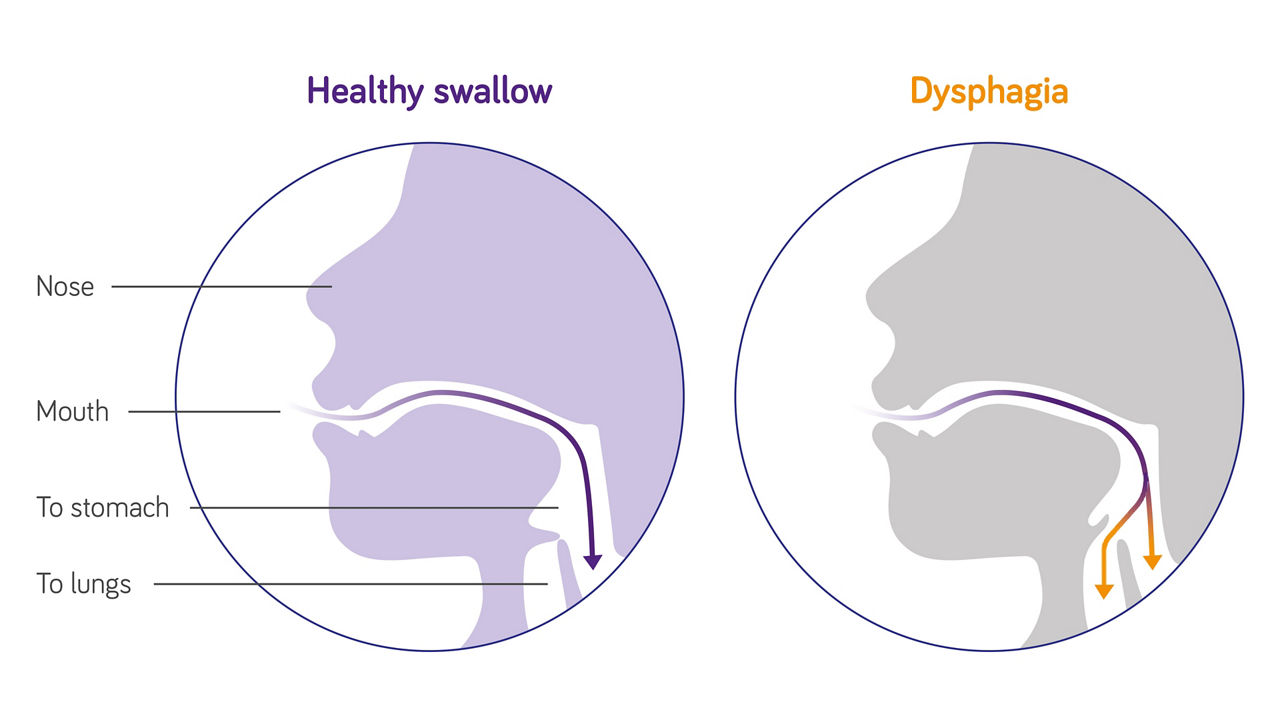
The risk to inhale food in the lungs (“aspiration”) due to dysphagia can be managed by starting what’s known as a ‘texture-modified diet’, where foods and drinks are prepared to a consistency that’s easier and safer to swallow. Many may find such meals and drinks unappetizing, so medical specialists may recommend using thickening agents to improve the texture of food and drink, without affecting taste. Specially pre-thickened products might also offer a more convenient source of nutrition and could help to prevent malnutrition. In addition, there are groups like the Chef’s Council, working hard to create recipes specific to the needs of dysphagia patients that are not only safe and nutritious, but appetizing and visually appealing too!
What can you do besides a texture-modified diet?
Besides diet modification, a change in posture or manoeuvres to direct food away from the weak site can be used to manage dysphagia. Furthermore a therapist can help teach exercises and techniques to strengthen the mouth, tongue and throat. A relatively new treatment is neurostimulation to improve the functioning of brain areas which are necessary for proper swallowing.
How long does dysphagia last after stroke?
Around half of all cases display dysphagia in the weeks following a stroke. For most patients, symptoms resolve within 6 months. For other patients, whose stroke may have been more severe, dysphagia can be a life-long condition.