How can nurses contribute to optimal nutritional care in cancer?
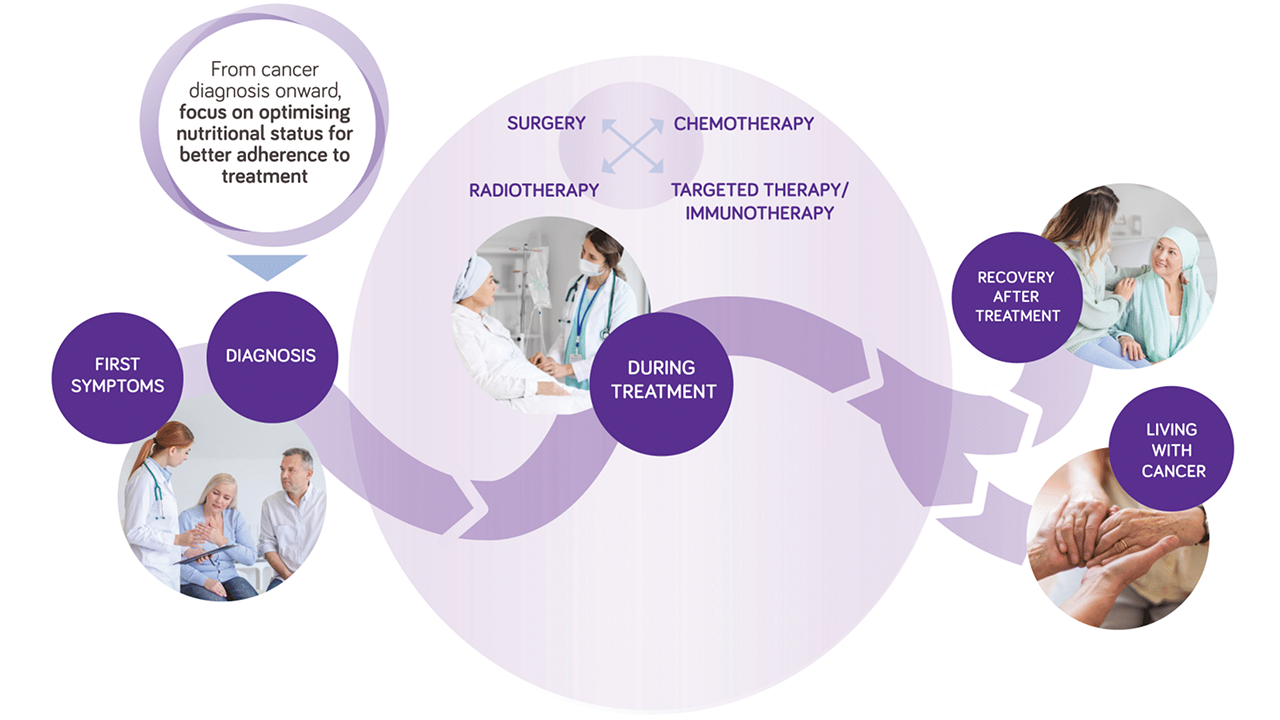
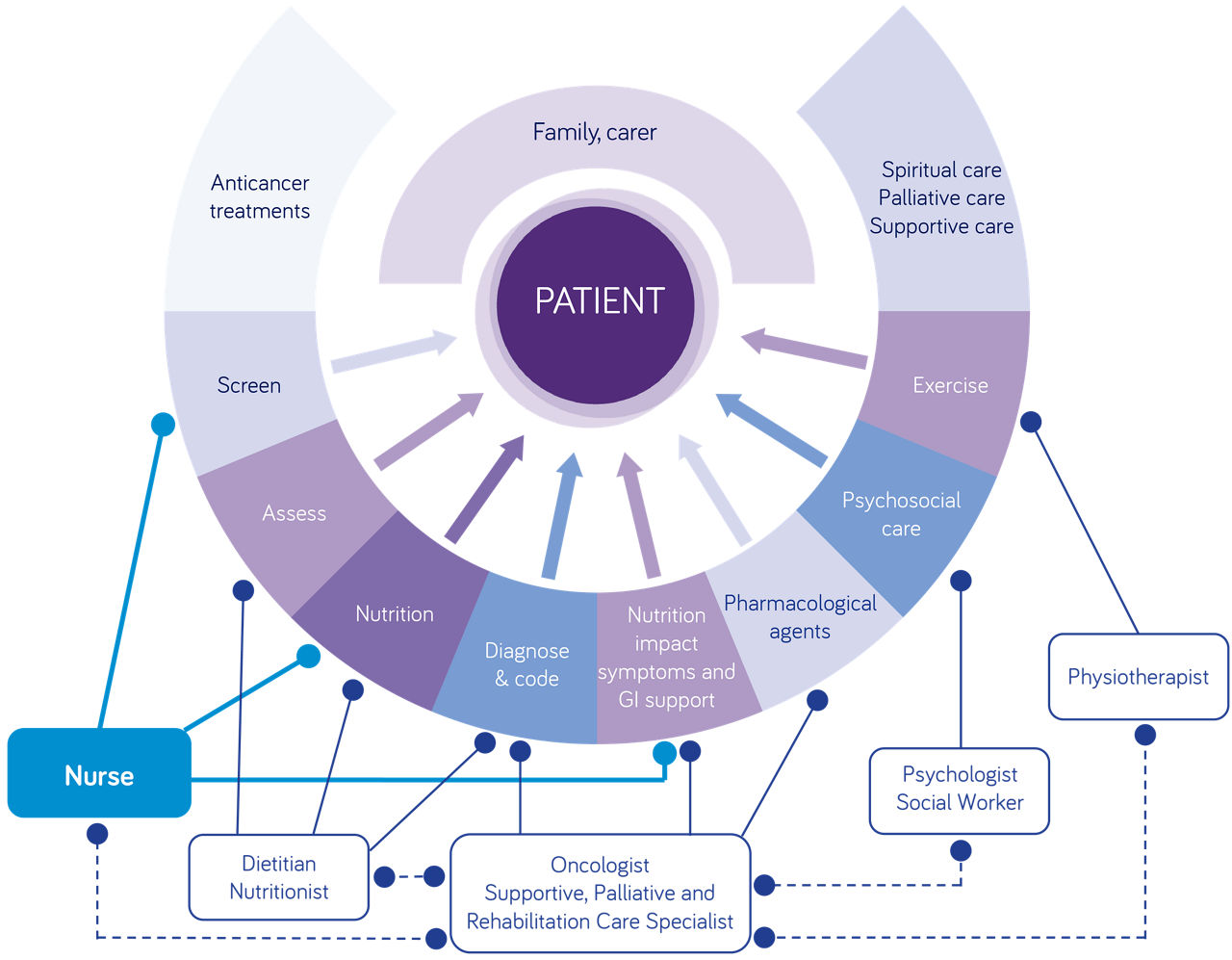
The nutrition care process can be described as a few-step process, from screening and assessment of malnutrition to interventions, monitoring and evaluation. Cancer nurses are in a great position to provide support and tailored information for patients with cancer on how to manage nutrition-related challenges through whole journey.
During cancer treatment, patients may develop side effects (such as taste & smell alterations) that have a negative effect on their ability to eat. Oncology nurses can inform patients according to nutritional guidelines , provide nutritional advice , promote self-management, psychosocial support, patient education and coaching. They can , also raise and discuss nutritional issues with the oncologist and the medical team.
Nutritional screening
To facilitate early identification of nutritional issues, nurses can implement validated malnutrition screening tool that can be used at each patient visit to help identify malnutrition risk at its earliest and most treatable stage. Examples of validated tools include the Malnutrition Screening Tool, NRS-2022, amongst others. Screening is an easy step to implement before conducting nutritional assessment to define patient needs and management strategies.
Nutrition therapy should be an integrative part of cancer care. Oncology nurses have a key role to play in discuss nutritional issues and ensure they are addressed with adequate nutritional advice, nutritional interventions and referral to a dietitian or nutritionist.
Useful resources
Please find below a useful list of resources to inform nurses on nutritional management in cancer: